
Allegiance Benefit Plan Management (Allegiance) is the third-party administrator (TPA) for Erlanger
Health System and is responsible for processing your employee health plan claims, answering your questions,
and helping you make the most of your health benefits. As a wholly-owned subsidiary of Cigna, we can offer
industry-leading flexibility and personalization, including access to Cigna's Open Access Plus provider network
for services unavailable at Erlanger Health System.
It is important to note, that while the Cigna Open Access Plus network is being utilized, benefits and services
are managed directly through Allegiance. Your Allegiance customer service team is here at 855-999-1527
to answer any questions about your Health Plan including benefits, claims status, enrollment and eligibility, and more.
Your providers should also contact Allegiance for any questions related to your benefits and claims.
Better Health Benefits
Start with Allegiance
Since 1981, the Allegiance Companies have earned a reputation for quality,
service, and efficiency unmatched throughout the country. Since its earliest days, our company has
been a leader in providing health benefit plans to employer groups and plan participants throughout
the United States.
We have always remained dedicated to one thing: outstanding customer service. That commitment continues today as strong as ever.
Our corporate spirit has always been one of allegiance to the companies we serve. Our people are deeply committed to our clients
and to plan participants.
Resources for Members
Health Forms
- Accident Questionnaire
- Authorization to Release Confidential Health Claim
- Alternate Payee Request Form
- Coordination of Benefits Questionnaire
- Submit a Medical Claim
- Request an ID Card
- Request for Services at Non-Erlanger Facility
- Standard Pre-Treatment Request (prior auth)
- Inpatient Admission Pre-Treatment Request (prior auth)
- Continuity of Care
Videos
Please Note: The walkthrough video reflects general login instructions. Please continue to log in using the login link on this custom site.
Take Allegiance On the Go
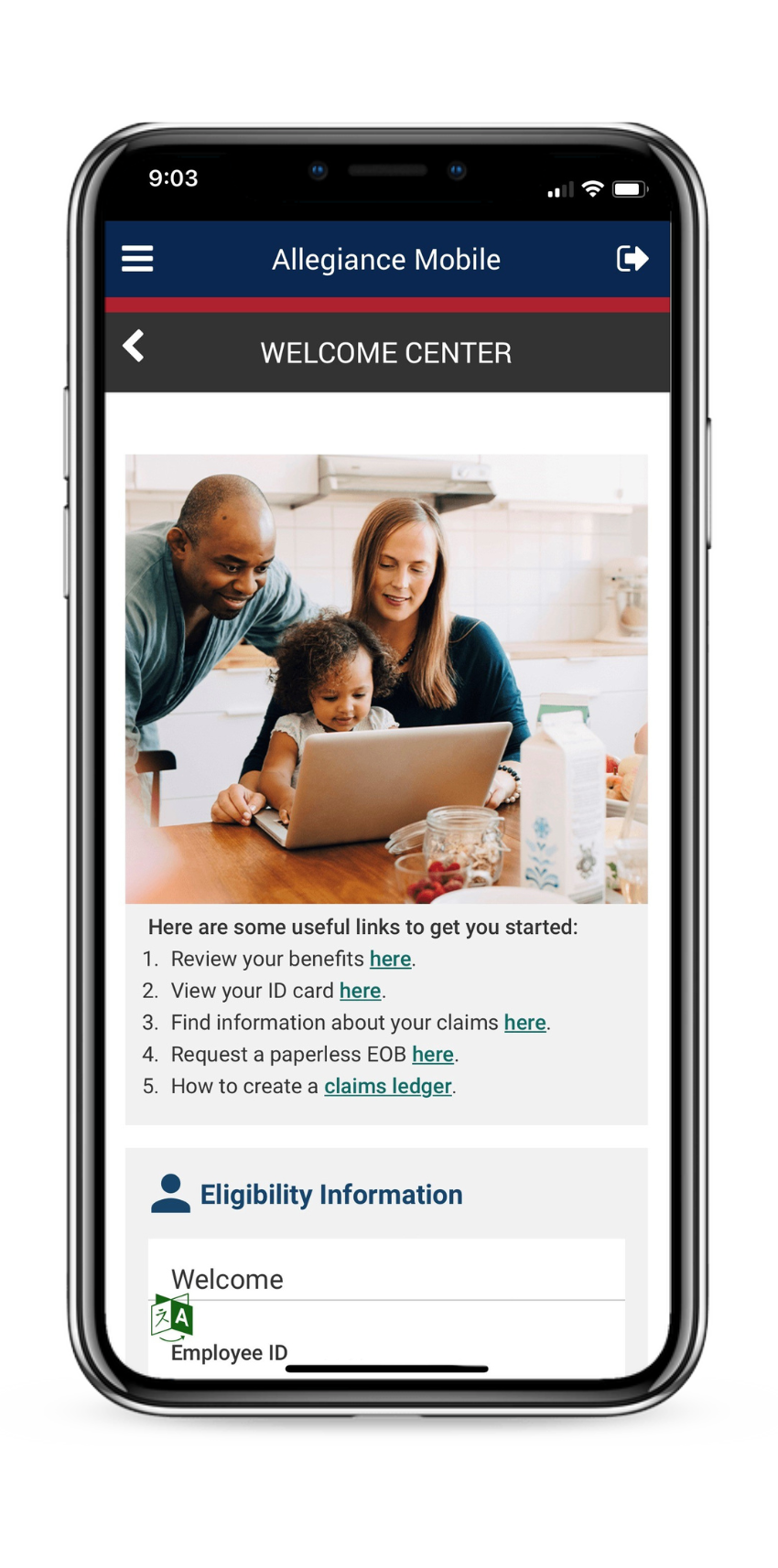
Our website offers personalized services at the click of a mouse. By registering, you will have 24
hour access to information regarding your health plan. You can check the status of a claim, review coverage
and benefits, and verify who is covered under your plan.
These services are also available through the Allegiance Mobile App available in Google Play and Apple App
stores.
Contact Us
PO Box 21074
Eagan, MN 55121
8:00 am - 8:00 pm EST
Customer Service 1-855-999-1527
Allegiance Holiday Closures
| New Year's Day | Thursday, January 1 |
| Martin Luther King Jr. Day | Monday, January 19 |
| Memorial Day | Monday, May 25 |
| Independence Day | Friday, July 3 |
| Labor Day | Monday, September 7 |
| Thanksgiving Day | Thursday, November 26 |
| Day after Thanksgiving | Friday, November 27 |
| Christmas Day | Friday, December 25th |
Notice
For assistance regarding a claim or to pre-notify for medical services,
please call the customer service number at 1-855-999-1527.
CAA Customer Balance Billing Disclosure Out-of-Network

